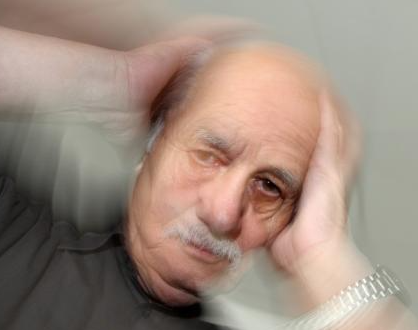
Ah, the simple act of standing up. You’ve been doing it since you were about a year old. It should be second nature. So why, in your 50s, 60s, and beyond, does it sometimes come with a bizarre, private light show? You push yourself up from your favorite armchair after a thrilling episode of your favorite crime drama, and suddenly, the room doesn’t quite look right. It’s not spinning, exactly. It’s more like a swarm of dark, fuzzy spots dancing at the edges of your vision, or a subtle graying-out of the world.
If this is your experience, welcome to the club. It’s a big one. And your first thought might be, “Whoa, that was weird. Maybe I stood up too fast.”
You’re right. But the real story behind those fleeting dark spots is a fascinating, and slightly dramatic, tale of plumbing, gravity, and a valiant effort by your body to keep you in the game. So, let’s pull back the curtain on this peculiar phenomenon.
The Gravity of the Situation: Your Body’s Uphill Battle
Let’s call those dark spots what they often are: a classic case of orthostatic hypotension. That’s a five-dollar term for a simple concept. “Orthostatic” means standing up, and “hypotension” means low blood pressure. Put them together, and you get “low blood pressure upon standing.”
Think of your circulatory system as a highly sophisticated, 60,000-mile-long plumbing network. Your heart is the magnificent, muscular pump. When you’re lying down or sitting, this system has it easy. Gravity is working on your entire body fairly equally, and your heart can merrily send blood to your brain with minimal opposition.
Now, stand up. Whoosh! Gravity immediately pulls about a pint of blood down into your legs and lower body. It’s like tipping a glass of water vertically; the liquid rushes to the bottom. For a brief moment, there’s less blood returning to your heart. Less blood in means less blood out. Your heart’s output drops.
This is a problem. Your brain, the brilliant but demanding command center, is at the top of the body. It is not a fan of interruptions in its blood supply. Blood carries the oxygen and glucose it needs to function. Even a few seconds of shortage can cause symptoms.
So, when that pint of blood pools in your legs, your brain sends out an urgent memo: “Hello?! We’re losing signal up here!”
The Emergency Broadcast System: How Your Body Responds
This is where the magic happens. Your body is equipped with a brilliant, automatic emergency response team. The moment it detects that drop in upper-body blood pressure, it springs into action.
- The Baroreceptors Sound the Alarm: Nestled in the major arteries near your heart and neck are tiny sensors called baroreceptors. They are the pressure gauges of your body. They instantly detect the dip in pressure and scream, “Mayday! Mayday! Pressure dropping!”
- The Sympathetic Nervous System Kicks In: This is your “fight or flight” system. Upon receiving the alarm, it orders your blood vessels, particularly the large ones in your legs and abdomen, to constrict tightly. Imagine stepping on a garden hose—the same amount of water flows through with much greater force. This vasoconstriction is your body’s way of stepping on the hose to push blood back up to your brain.
- Your Heart Joins the Fray: At the same time, your heart gets the command: “Beat faster and harder!” It revs up, trying to increase output to overcome the gravitational challenge.
This entire, complex sequence happens in a heartbeat (pun intended). When it works perfectly, you stand up and feel… perfectly normal. You are blissfully unaware of the heroic internal effort that just took place.
But when the response is a little too slow, or a little too weak, you get the light show. Those dark spots or tunnel vision are quite literally your brain experiencing a momentary, minor oxygen debt. It’s your visual cortex saying, “We’re running on backup power here, people!” The slight dizziness is the rest of the brain chiming in. It usually lasts just a few seconds—just long enough for your body’s emergency team to catch up and restore full pressure.
So, Why Now? The Plot Thickens with Age
If this is a new or more frequent guest in your life, you’re probably wondering why. You didn’t used to have this issue after standing up from your beanbag chair in your 20s. What’s changed?
Aging, as it turns out, adds a few twists to our tale.
- Stiffer Pipes: As we get older, our arteries can become less flexible and more resistant to the “constrict now!” command from the nervous system. They’re a bit slower to clamp down, allowing blood to linger in the legs a moment longer.
- A More Leisurely Pump: The baroreceptors themselves can become less sensitive. They might be a bit slower to sound the alarm, creating a tiny delay in the entire response.
- Hydration Habits: This is a big one. Our sense of thirst often diminishes with age. We might not drink as much water as we used to, leading to mild, chronic dehydration. Less water in your system means less blood volume, which makes you far more susceptible to pressure drops. It’s like trying to run water through a system with a half-full tank.
- Medication Side Effects: The plot thickens! Many common medications can contribute to orthostatic hypotension. Blood pressure medications (especially diuretics, or “water pills”), medications for an enlarged prostate (alpha-blockers), some antidepressants, and even nitrates for heart pain can all relax blood vessels or reduce blood volume, exacerbating the problem.
- The Crossover Conundrum: For men, an enlarged prostate can mean more frequent trips to the bathroom at night. This, combined with perhaps a diuretic medication, can lead to dehydration by morning, making those first steps out of bed a particularly wobbly affair.
Beyond the Spots: Should You Be Worried?
For the vast majority of people, occasional orthostatic hypotension is more of an annoyance than a dire emergency. It’s your body’s way of saying, “Hey, take it easy. Let me do my job.”
However, it’s important to listen to the nuances of the message. You should definitely have a chat with your doctor if:
- The episodes are frequent and not improving with simple measures.
- You actually lose consciousness or fall. This is a red flag.
- The symptoms last for more than a minute or two.
- It’s accompanied by chest pain, confusion, or shortness of breath.
Your doctor can perform a simple “tilt test” (checking your blood pressure and heart rate while lying down and then standing) and review your medications and health history to rule out other causes.
Becoming the Hero of Your Own Story: Simple Hacks to Beat the Drop
The good news is that you are not a passive passenger in this process. You can train your body’s response and make simple lifestyle changes that can dramatically reduce these episodes. Think of it as upgrading your internal plumbing and fine-tuning the emergency response team.
- The Slow-Motion Director: Don’t jump up. Ever. When waking up, spend a minute sitting on the edge of the bed. Wiggle your toes, pump your ankles. Then stand up, holding onto something stable if needed. Do the same when rising from a chair: move to the edge, move your feet around for a few seconds, then push up steadily.
- The Hydration Hero: This is your superpower. Make a conscious effort to drink water throughout the day. Don’t wait until you’re thirsty. Keep a water bottle handy. If you take a diuretic, talk to your doctor about the best timing for your water intake. Sometimes, a single large glass of water first thing in the morning can provide a helpful volume boost.
- The Leg Pump Maneuver: Before you stand, engage your leg muscles. Repeatedly clench and unclench your thigh and calf muscles. Your leg muscles are often called your “second heart” because when they contract, they squeeze the veins and help push blood back upward. Crossing and uncrossing your legs while sitting can also help.
- Avoid the Triggers: Large, high-carb meals can sometimes cause blood to rush to your digestive system, diverting it from the brain. So, be mindful after a big lunch. Alcohol and hot weather can also dilate blood vessels and worsen the problem.
- Compression Socks – Your Secret Weapon: Don’t scoff! These aren’t just for long flights. Well-fitting compression socks apply gentle pressure to your legs, making it harder for blood to pool there in the first place. They give your circulatory system a head start.
- Stay Salty? (With a Caveat): For some people with low blood pressure, a slightly higher salt intake can help retain fluid and increase blood volume. BUT—and this is a huge but—do not do this without consulting your doctor, especially if you have high blood pressure or heart or kidney conditions.
So, the next time you stand up and the world briefly goes fuzzy and spotty, don’t just shrug it off. Smile. You’ve just witnessed a brief, dramatic performance starring your own body. It’s a reminder of the incredible, automatic systems working 24/7 to keep you upright and aware. It’s not a sign of failure; it’s a sign of a system adapting, a testament to the long and fascinating journey of your body through time. And with a few simple tricks, you can help it run the show a little more smoothly. Now, take a sip of water and go enjoy your day.